Smoking vessels: Symptoms, reasons, and remedies for damaged blood vessels
Blown veins, a common complication during medical procedures, occur when a vein is damaged due to a needle puncture, causing it to leak blood into the surrounding area. This article explores the causes, symptoms, and treatment methods associated with blown veins.
**Causes:**
Vein or capillary rupture can occur due to vein fragility, improper needle insertion, overfilling veins with fluid, or anticoagulant use that affects blood clotting. Chronic conditions such as varicose veins, deep vein thrombosis (DVT), or chronic venous insufficiency can lead to vein weakening or rupture. Other contributing factors include age-related vessel fragility, high blood pressure, trauma or excessive pressure on veins, and medications that impair clotting like blood thinners. Environmental factors such as extreme temperature changes and sun exposure may also cause superficial capillaries to break, especially in the face.
**Symptoms:**
Visible signs of a blown vein include swelling and discoloration under the skin where the vessel burst, often appearing as bruising or red, blue, or purple lines (broken capillaries). Pain or tenderness may accompany the swelling. In more severe venous issues, symptoms like leg ulcers, chronic swelling, and heaviness may develop. In procedural settings, immediate bruising or hematoma near the needle site may be noticeable.
**Treatment Methods:**
Treatment depends on severity, location, and cause. Conservative treatments include compression therapy (e.g., compression socks) to reduce swelling and pain, improve circulation, and prevent further vein damage. Anti-inflammatory medications may be used to manage pain and swelling. Lifestyle changes such as leg elevation, exercise, and weight management can improve blood flow and venous health.
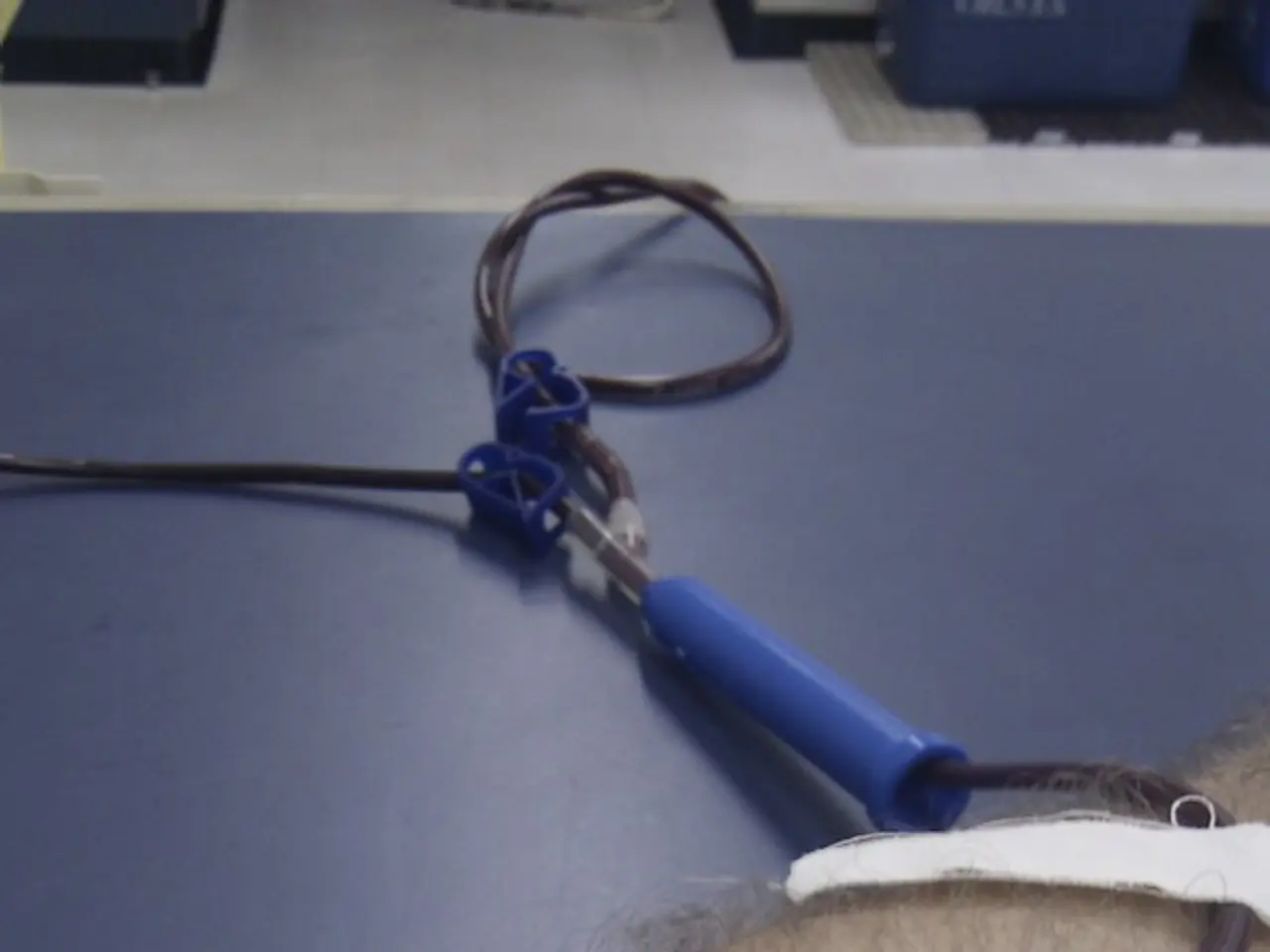
Minimally invasive procedures like sclerotherapy, endovenous thermal ablation, and Veinwave (thermal coagulation) are also options. Sclerotherapy involves injecting a solution into the affected vein, causing it to scar and close, with blood rerouted through healthier veins. Endovenous thermal ablation uses radiofrequency or laser heat to close problematic veins. Veinwave applies targeted heat to collapse small broken veins, especially facial capillaries, allowing natural reabsorption.
Surgical interventions such as vein stripping and ligation, endoscopic vein surgery, and stenting may be necessary in advanced cases.
**Additional Notes:**
Some topical creams like retinoids may thicken skin to reduce the visibility of superficial veins but do not eliminate the veins themselves. Temporary cosmetic camouflage is possible but does not address the underlying vein damage. Preventive care and careful technique during medical procedures reduce the risk of blown veins.
It is essential to inform a doctor or nurse if a person's veins have ruptured in the past to help prevent blown veins. Using wound dressings that keep the insertion site visible, stabilizing the individual during needle insertion, and good communication between medical professionals and individuals they treat can also help avoid blown veins.
If a person using an IV line at home notices signs of infiltration, such as swelling, pain, or discoloration, they should contact a doctor immediately. Quick treatment is crucial to prevent complications like extravasation, which occurs when a drug that causes irritation seeps into the tissue surrounding a blown vein.
In conclusion, blown veins are a common complication during medical procedures that can be prevented with proper care and technique. Understanding the causes, symptoms, and treatment methods associated with blown veins is crucial for both medical professionals and individuals receiving treatments to ensure the best possible outcomes.
- While age-related vessel fragility can contribute to blown veins, certain chronic conditions such as type 2 diabetes, bipolar disorder, or ulcerative colitis may also cause vein weakening or rupture.
- Chronic medical conditions like multiple sclerosis, dermatitis, or atopic dermatitis can lead to skin issues that require medical procedures, increasing the risk of blown veins.
- Similarly, individuals managing conditions like HIV, breast cancer, or non-small cell lung cancer (NSCLC) may be susceptible to blown veins due to frequent treatments or procedures.
- Additionally, people living with obesity might experience extra pressure on their veins, increasing the risk of blown veins during medical procedures or daily Activities.
- Some autoimmune diseases, such as rheumatoid arthritis or ankylosing spondylitis, can lead to joint inflammation and pain, potentially resulting in the need for medication that impairs clotting, thereby increasing the risk of blown veins.
- Individuals managing migraines may undergo procedures requiring vein puncture, hence being at risk for blown veins.
- Preventive measures for blown veins are essential in maintaining health-and-wellness, especially for those with multiple medical conditions like depression, Crohn's disease, and HIV.
- Skin care is equally important, as sun exposure or extreme temperature changes may cause superficial capillaries to break, leading to blown veins, particularly on the face.
- While scientific advancements have led to predictive analysis in medical conditions like diabetes or skin disorders, more research is needed to develop reliable methods for identifying an increased risk of blown veins among different populations.
- It is crucial to consider the factors that influence blown veins when discussing health-and-wellness, particularly when addressing medical-conditions and skin care.
- Understanding the connection between blown veins and various medical conditions can aid healthcare professionals in making informed decisions about treatment methods and overall care.
- Proper education about the risk factors, symptoms, and treatment options associated with blown veins can help individuals better manage their health, especially when dealing with multiple medical conditions.
- Collaboration between researchers, healthcare professionals, and individuals managing various medical conditions can lead to improved blown vein prevention, treatment, and increased understanding of this common complication in medical practices.