Liver Cirrhosis Patient Undergoes Vascular Embolization for Mesenteric Arteriovenous Malformation, Resulting in Lowered Portal Pressure - A Case Study Report
A 66-year-old man, with a medical history of fatty liver, hypertension, hyperuricemia, and chronic gastritis, was diagnosed with portal hypertension due to an arteriovenous malformation (AVM) in the mesentery. The patient's chief complaint was fatigue, and he also exhibited hepatic dysfunction as shown by blood tests.
Upon examination, no abnormalities were seen. However, on abdominal ultrasound, signs of cirrhosis and splenomegaly were observed in the liver, with no ascites. On abdominal contrast-enhanced computed tomography, blunting of the liver edge and splenomegaly were confirmed, and an anastomosis of the ileal artery and ileal vein via a nidus within the mesentery was identified.
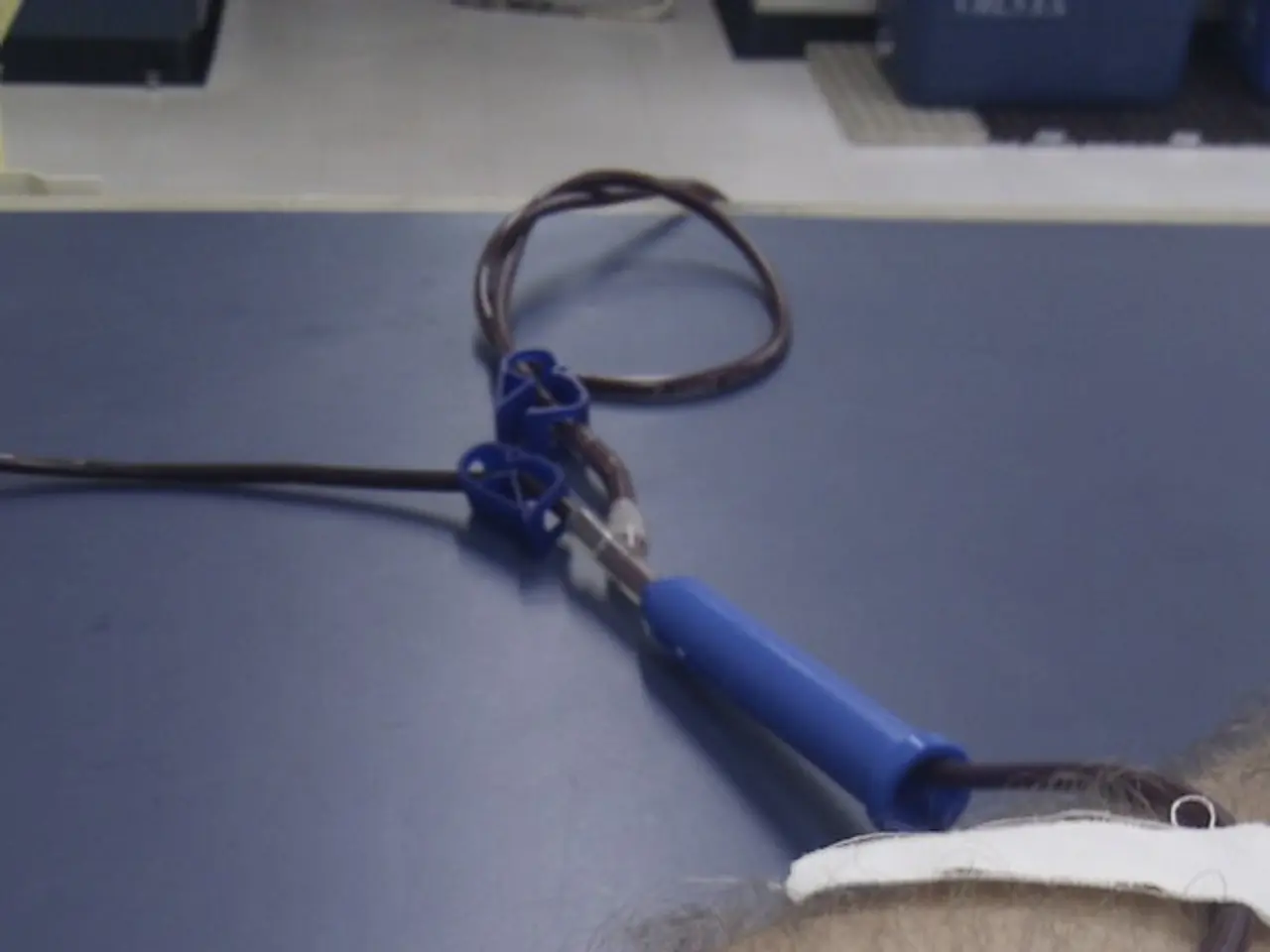
The ileal vein, which was the dominant outflow vein, was embolized, causing the blood flow in the AVM to disappear. Vascular embolization with a percutaneous transhepatic approach was performed for the mesenteric AVM. Fortunately, there were no complications from the embolization.
Table 1 shows the patient's laboratory test results. A decrease in portal pressure of 29% was confirmed following the embolization. The patient tested negative for hepatitis B, hepatitis C virus, and antinuclear and antimitochondrial antibodies.
Percutaneous transhepatic vascular embolization (PTVE) for treating mesenteric AVMs that contribute to portal hypertension offers a minimally invasive alternative to surgical intestinal resection. This procedure involves catheter-based occlusion of abnormal blood vessels to reduce shunting and relieve portal pressure, thereby addressing the hemodynamic cause of portal hypertension without removing intestinal tissue.
Effects and Potential Benefits of PTVE Compared to Surgical Intestinal Resection
PTVE offers several advantages over surgical intestinal resection. A minimally invasive approach means less operative trauma, reduced risk of infection, shorter hospital stays, and quicker recovery. By embolizing the aberrant arterial feeders or venous outflow pathways of the AVM, PTVE directly reduces abnormal high-flow shunting, which can lower portal hypertension and prevent related complications such as variceal bleeding or ascites. Moreover, embolization does not remove bowel segments, thereby avoiding potential complications like short bowel syndrome, malabsorption, or surgical adhesions. Embolization can be repeated if necessary or combined with other interventions such as transjugular intrahepatic portosystemic shunt (TIPSS) for complex cases of portal hypertension.
Limitations and Considerations
Despite its benefits, PTVE has its limitations. There may be a risk of AVM recanalization or recruitment of collateral vessels after embolization, potentially requiring multiple procedures or complementary surgeries. Technical complexity demands careful angiographic mapping and embolic agent selection to avoid non-target embolization and ischemia of healthy bowel. Surgery remains definitive for symptomatic or complicated AVMs, especially those causing bowel ischemia, bleeding, or significant mass effect. Also, resection may be preferable when embolization is technically infeasible or has failed.
Overall Comparison
| Aspect | Percutaneous Transhepatic Embolization | Surgical Intestinal Resection | |-------------------------------|--------------------------------------------------|-----------------------------------------------| | Invasiveness | Minimally invasive catheter procedure | Major abdominal surgery | | Recovery time | Shorter hospital stay, faster recovery | Longer hospitalization, slower recovery | | Bowel preservation | Entire bowel preserved | Segmental bowel removed | | Risk of complications | Vascular injury, incomplete embolization | Surgical risks, adhesion, short bowel syndrome | | Potential for repeat therapy | Yes, can be repeated or combined with other treatments | Usually single intervention | | Definitive cure | May require multiple embolizations; possibility of recurrence | Often definitive if all abnormal tissue resected |
Given these factors, PTVE is increasingly favored as the first-line treatment for mesenteric AVMs causing portal hypertension when technically feasible, offering potential benefits in safety, recovery, and bowel preservation compared to surgical resection. However, surgery remains critical in selected cases with complications or failed embolization. Further comparative studies are needed to establish long-term outcomes between these approaches definitively.
This report details a case in which portal pressure was decreased by percutaneous transhepatic vascular embolization of an idiopathic mesenteric AVM. Endovascular treatment, which is less invasive compared to surgical intestinal resection, is thought to be a possible option for treating mesenteric AVMs. The patient regularly consumes about 100-180 g per day of alcohol, but no significant alcohol-related liver disease was observed.
The patient's medical history includes fatty liver, hypertension, hyperuricemia, chronic gastritis, and recently diagnosed chronic kidney disease due to an arteriovenous malformation (AVM) in the mesentery. To treat the mesenteric AVM, the ileal vein was embolized, and percutaneous transhepatic vascular embolization (PTVE) was performed.
The benefits of PTVE in this context include fewer surgical risks, reduced recovery time, and the preservation of bowel segments. However, potential complications might arise from AVM recanalization, collateral vessel recruitment, or vascular injury due to incomplete embolization.
In cases of complications or when embolization is infeasible, surgical intestinal resection might still be necessary. Although the patient regularly consumes alcohol, no significant alcohol-related liver disease was observed.
To improve workplace-wellness and manage chronic-diseases, employees can adopt health-and-wellness practices like fitness-and-exercise, skin-care, nutrition, and weight-management. Moreover, the use of cannabidiol (CBD) as a potential treatment for various medical-conditions, such as anxiety and chronic pain, is a growing area of interest in the field of science.
In light of the patient's case, endovascular treatment seems to be a viable option for managing mesenteric AVMs, offering less invasiveness compared to surgical intestinal resection.